Connect With Us

Suggested Foot Care For Diabetic Patients

Diabetes can pose significant risks to foot health due to potential nerve and blood vessel damage. Reduced sensation in the feet increases the likelihood of injuries, which may lead to serious complications like foot ulcers, often requiring hospitalization. It is important for anyone with diabetes to prioritize foot care to prevent such issues. Daily foot inspections are vital, checking for dry skin, blisters, sores, bruises, and any abnormalities. Regular washing with mild soap, careful drying, and moisturizing are also essential steps. Proper toenail trimming techniques help to prevent ingrown nails and other complications, with assistance from a podiatrist recommended for thick or discolored nails that may be infected. Corns and calluses should also be managed by a podiatrist, ensuring safe removal. Wearing well-fitting shoes and clean, dry socks are recommended at all times to prevent injuries. Any foot issues should be promptly reported to a podiatrist, rather than attempting self-treatment. It is suggested that diabetic patients seek assistance from a podiatrist for regular evaluations and necessary foot care.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Rahil Baxamusa, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.
The Relationship Between Arthritis and Bunions

Arthritis, encompassing various inflammatory conditions, can contribute to bunion formation, affecting the feet in distinct ways. A bunion, characterized by a bony protrusion at the base of the big toe, often results from joint misalignment. Types of arthritis such as rheumatoid arthritis, osteoarthritis, psoriatic arthritis, and gout can all play a role in its development. Rheumatoid arthritis induces joint damage and inflammation, leading to joint instability and eventual bunion formation. Osteoarthritis contributes by wearing down cartilage, promoting joint misalignment. Psoriatic arthritis, a condition linked to psoriasis, can also cause bunion formation, often accompanied by inflammation in toes. Additionally, gout, characterized by sudden, intense joint pain, commonly targets the big toe joint, potentially leading to bunion development. A podiatrist's involvement is important in managing arthritis-related bunions. They can provide personalized treatment plans, including pain management strategies, footwear recommendations, custom orthotic devices, and surgical options if necessary, ensuring optimal foot health and mobility. If you have a painful bunion, it is suggested that you schedule an appointment with a podiatrist who can help you to manage this and other arthritis-related foot conditions.
If you are suffering from bunions, contact Rahil Baxamusa, DPM of Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Osteoporosis and Fractures of the Feet

Osteoporosis isn't just about fragile bones. It can impact balance, leading to falls and injuries beyond just the ankle and foot. Even without a specific foot or ankle injury, you might notice pain and swelling in these areas, signaling potential bone issues. Several factors contribute to the likelihood of developing osteoporosis, some within your control and others not. Age is a significant factor, with the risk rising notably for women over 50 and men over 70. Women are more predisposed to osteoporosis and genetics can further increase the risk. While you can't change your age, gender, or genetics, certain lifestyle factors help to reduce your risk. A balanced diet rich in essential nutrients helps maintain bone strength. Hormonal changes, such as low estrogen levels in women and testosterone in men, can affect bone mass and should be monitored. Excessive alcohol consumption and smoking can weaken bones and overall health. Regular exercise, especially weight-bearing activities, can strengthen bones and improve bone density. Even moderate daily exercise, like taking a walk, can make a significant difference in bone health. By understanding these factors and making informed choices, you can take proactive steps to protect your bone health and minimize the risk of osteoporosis-related complications in your feet. If you are experiencing foot or ankle pain that may be connected to osteoporosis, it is suggested that you make an appointment with a podiatrist for an exam and treatment options.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Rahil Baxamusa, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
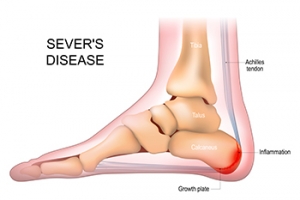
Sever’s Disease and Children’s Heel Pain
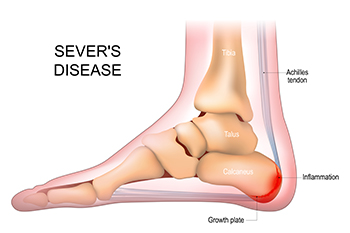 Sever's disease, also known as calcaneal apophysitis, is a common cause of heel pain in growing children and adolescents, especially in those who play sports. This condition occurs when the growth plate in the heel becomes inflamed, often due to repetitive stress from activities like running and jumping. This, combined with the pressure of rapid bone growth during puberty, can create painful heels. The pain may worsen during or after physical activity and include tenderness to the touch. It may also lead to limping, especially after waking up or more intense physical activities. Treatment typically involves rest and various exercises that stretch and strengthen the leg muscles and tendons. Footwear with proper cushioning and support is also suggested to help alleviate symptoms. With appropriate management, symptoms usually resolve with the completion of the growth spurt, as the heel bone matures. If your child has painful heels and you suspect Sever’s disease, it is suggested that you make an appointment with a podiatrist for a diagnosis and management techniques.
Sever's disease, also known as calcaneal apophysitis, is a common cause of heel pain in growing children and adolescents, especially in those who play sports. This condition occurs when the growth plate in the heel becomes inflamed, often due to repetitive stress from activities like running and jumping. This, combined with the pressure of rapid bone growth during puberty, can create painful heels. The pain may worsen during or after physical activity and include tenderness to the touch. It may also lead to limping, especially after waking up or more intense physical activities. Treatment typically involves rest and various exercises that stretch and strengthen the leg muscles and tendons. Footwear with proper cushioning and support is also suggested to help alleviate symptoms. With appropriate management, symptoms usually resolve with the completion of the growth spurt, as the heel bone matures. If your child has painful heels and you suspect Sever’s disease, it is suggested that you make an appointment with a podiatrist for a diagnosis and management techniques.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Rahil Baxamusa, DPM from Illinois. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
Origins of Blisters on the Feet

Blisters on the feet can be an unwelcome nuisance, often causing discomfort and hindering mobility. These fluid-filled sacs typically form in response to friction or repetitive rubbing against the skin. When excessive pressure or irritation occurs, the outer layer of the skin separates from the underlying tissue, creating a protective bubble filled with fluid. Common culprits behind blister formation include wearing ill-fitting shoes, prolonged periods of walking or running, and friction caused by sweaty or damp conditions. Additionally, certain activities, such as hiking or wearing new shoes without proper breaking in, can increase the likelihood of developing blisters. Individuals with foot deformities or abnormalities may also be more prone to blister formation due to uneven pressure distribution. If you have a blister on your foot that has become infected, it is suggested that you consult a podiatrist who can safely treat it and provide effective prevention techniques for future knowledge.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Rahil Baxamusa, DPM of Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.