Connect With Us

Causes and Treatment of Achilles Tendon Pain

Achilles tendon pain can arise from various causes and often affects the area where the Achilles tendon inserts into the back of the heel. The Achilles tendon is the largest tendon in the body, connecting the calf muscles to the heel bone, and facilitating activities like walking, running, and jumping. Common causes of Achilles tendon pain include overuse or repetitive strain, resulting in conditions such as Achilles tendinitis or tendinosis. These conditions involve inflammation or degeneration of the tendon due to excessive stress. Acute injuries such as Achilles tendon ruptures can occur from sudden, forceful movements, and are often accompanied by a popping sensation and severe pain. Treatment for Achilles tendon pain typically involves rest, compression, and elevation, in addition to medicine to help reduce pain and inflammation. Stretching exercises and custom-made orthotic devices may be recommended to improve flexibility and strength, which can help to support the Achilles tendon. In severe cases or ruptures, surgery may be necessary to repair the tendon. If you have a painful Achilles tendon, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Rahil Baxamusa, DPM of Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Offloading Practice for Foot Wounds

Offloading practice for foot wounds refers to alleviating pressure and stress on injured or ulcerated areas of the foot. Offloading involves the strategic redistribution of weight to prevent further damage and promote healing. This method is particularly critical for individuals with diabetes or other conditions that affect circulation and reduce sensation in the feet. The essence of offloading lies in its ability to relieve pressure from vulnerable areas, allowing tissues to recover and regenerate without constant irritation or trauma. Offloading practice uses specialized footwear, orthotics, or other assistive devices to encourage healing and helps prevent wounds from getting worse. Additionally, it emphasizes the need for close collaboration between patients, caregivers, and podiatrists to optimize treatment outcomes. If you have diabetes and have a foot wound that has become ulcerated, it is strongly suggested that you are under the care of a podiatrist who can help you to manage this condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Rahil Baxamusa, DPM from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Are Bunions Affecting Your Everyday Life?
The Importance of Choosing the Right Running or Walking Shoe

Selecting the appropriate running or walking shoe is critical for both performance and injury prevention. The right shoe provides support, stability, and cushioning tailored to individual foot mechanics and activity level. Wearing the wrong shoe can lead to discomfort, pain, and even injury. For runners, factors such as pronation, which is the natural inward roll of the foot, arch height, and foot width should be considered when choosing footwear. Meanwhile, walkers should prioritize shoes that offer adequate cushioning and flexibility to accommodate the repetitive motion of walking. Wearing ill-fitting shoes can contribute to conditions like blisters, plantar fasciitis, shin splints, and stress fractures, that hinder progress and enjoyment. Investing in high-quality, properly fitting footwear is an investment in your foot health and overall well-being, ensuring comfort, support, and longevity as you pursue your fitness goals. If you have questions about what type of shoe to buy for you desired fitness routine, it is suggested that you confer with a podiatrist.
For more information about walking shoes versus running shoes, consult with Rahil Baxamusa, DPM from Illinois. Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Differences between Walking and Running Shoes
Both running and walking are great exercises, but should a person wear the same shoes for both activities? The answer is no, because there is a difference between the way a person’s feet hit the ground when they are walking and when they are running. Therefore, the shoes for each activity are designed differently. Before you begin any exercise program it is always recommended that you speak with your doctor or podiatrist.
Walking is a low impact exercise that is often recommended by doctors to their patients. While walking is a simple activity, it still requires some degree of preparation. If you think about walking and how your feet strike the ground as you move, you will notice that your heel hits the ground first before your foot continues to roll forward and your next step begins. Because of this rolling motion, walking shoes are designed to be more flexible than running shoes. This flexibility helps the walker push off with each step taken.
Because the heel hits the ground first when you walk, walking shoes are designed to absorb most of the shock. Walking shoes should therefore have a beveled or angled heel. The angle of the heel helps absorb the shock and reduces pressure from the ankles. This is especially important for speed walkers, as their feet will hit the ground twice as often as the normal walker.
When people decide to run as a hobby or for their health, they must first realize that running is a high impact exercise. If not done with the proper equipment, running may cause damage to the feet and legs. Running shoes are designed to be more lightweight and to have thicker soles. The thicker soles act as shock absorbers for the rest of the body. Walking shoes often do not have the proper arch support that running shoes do.
A proper fitting shoe can make or break a runner or a walker. If the shoes are too big, their feet will slide back and forth inside the shoe and cause blisters. Whether you will be running or walking, the right equipment can make all of the difference in the world.
Toe Pain May Be Caused by Sesamoiditis
The sesamoid bones of the feet are small yet significant structures embedded within tendons under the big toe. They play a vital role in joint stabilization and the ability to raise the toe. Sesamoiditis usually results from post-traumatic or degenerative causes, causing localized pain and swelling, with tenderness over the affected bones. Factors contributing to sesamoiditis include osteoarthritis, foot deformities, and high-impact activities. Other potential causes of sesamoiditis include wearing high heels, increased body weight, running on the forefoot, and a larger size of sesamoids. Treatment may include footwear modifications and orthotic shoe inserts. In severe cases, steroid injections or surgery may be necessary to alleviate symptoms and prevent further complications. Seeking a prompt evaluation by a podiatrist is essential. If you are experiencing persistent toe pain or suspect sesamoiditis, it is suggested that you schedule an appointment with a podiatrist for an exam, a diagnosis, and appropriate treatment options.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Rahil Baxamusa, DPM of Illinois. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
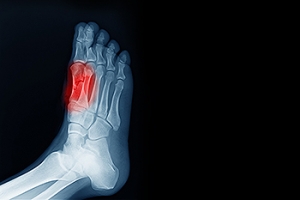
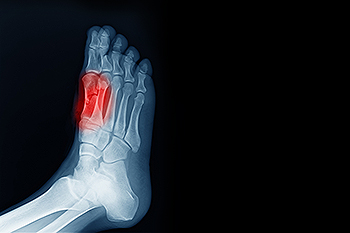
Signs and Symptoms of a Broken Foot
 The main symptoms of a broken foot are severe pain, swelling, and bruising around the injured area. Some patients may experience very intense pain when touching or applying pressure to the foot. Difficulty or inability to bear weight on the foot, along with visible deformities or changes in foot shape, can also indicate a potential break. Numbness of the foot is another possible symptom. X-rays or other imaging tests are commonly used to confirm the presence of a fracture. Taking immediate steps to address a potential broken foot can lead to a more effective recovery and prevent complications down the line. If you have a painful foot and suspect a break or fracture, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and appropriate treatment.
The main symptoms of a broken foot are severe pain, swelling, and bruising around the injured area. Some patients may experience very intense pain when touching or applying pressure to the foot. Difficulty or inability to bear weight on the foot, along with visible deformities or changes in foot shape, can also indicate a potential break. Numbness of the foot is another possible symptom. X-rays or other imaging tests are commonly used to confirm the presence of a fracture. Taking immediate steps to address a potential broken foot can lead to a more effective recovery and prevent complications down the line. If you have a painful foot and suspect a break or fracture, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and appropriate treatment.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Rahil Baxamusa, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.