Connect With Us

Wound Debridement

The removal of dead or infected skin tissue is known as debridement. This procedure also eliminates foreign materials from tissue. Debridement promotes the growth of healthy tissue, minimizes scarring, and reduces infection complications. Not all wounds require debridement. It is typically used for non-healing old wounds, chronically infected wounds, or those at risk of infections. Severe or new wounds might also need debridement. The choice of debridement depends on factors like wound type, age, overall health, and risk for complications. Methods include biological debridement using sterile maggots, enzymatic debridement with ointments, autolytic debridement harnessing the body's enzymes, and mechanical debridement as the most common approach. Sharp debridement, both conservative and surgical, involves cutting off unhealthy tissue. Recovery varies but typically takes 6 to 12 weeks. Careful wound management, including regular dressing changes and hygiene, is crucial. Although complications are possible, debridement's benefits often outweigh the risks. If you have a foot wound that persists or appears infected, it is strongly suggested that you see a podiatrist for immediate treatment, which might include debridement.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Rahil Baxamusa, DPM from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
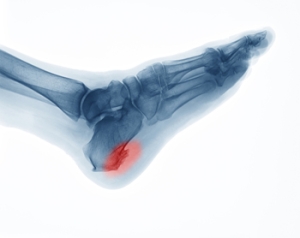
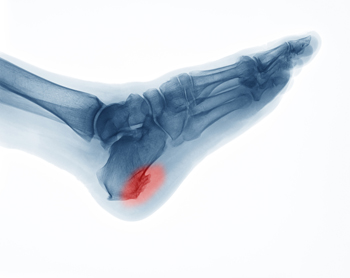
Common Myths About Heel Spurs
Heel spurs are commonly misunderstood and usually do not cause heel pain. In fact, most heel pain is attributed to plantar fasciitis, a condition where the ligament on the bottom of the foot, termed the plantar fascia, becomes chronically inflamed. It then can get calcified where it attaches to the heel bone. It may even appear as a heel spur on an X-ray. The pain stems from the strain on the plantar fascia, due to overuse or repetitive exertion, and often is made worse by wearing inadequately supportive footwear. Symptoms include discomfort on the bottom of the heel, which occasionally extends into the arch. Surgical removal of heel spurs is largely considered unnecessary, as relief from the pain can often occur without addressing the spur itself. Wearing shoe inserts and incorporating simple stretches can lead to significant relief from this type of heel pain. Proper arch support and cushioning are often effective ways to relieve heel pain. So, while heel spurs may appear concerning, they may not be the main cause of discomfort. Instead, it is suggested that you make an appointment with a podiatrist who can conduct imaging tests and identify the cause and suggest the appropriate treatment measures.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Rahil Baxamusa, DPM from Illinois. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Crystal Lake, IL . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Reasons for Cracked Heels

Mildly cracked heels are generally not a serious foot condition unless they develop into fissures, which may bleed and become infected. Cracked heels are caused by standing on hard or uneven surfaces for most of the day, or from wearing shoes that do not have a back. Flip-flops fall into this category, and it is beneficial to limit wearing these types of shoes. Patients who have existing medical conditions, such as psoriasis, diabetes, or a thyroid disorder, may be prone to getting cracked heels. One of the first signs that cracked heels may be developing is the hard, thickened skin surrounding the heel. This is referred to as a callus and can be yellow or brown in color. Cracks can form over the callus and can become worse when pressure of standing or running is exerted. Effective prevention methods can include washing and drying the feet daily, followed by applying a good moisturizer on them. If you have cracked heels that are causing problems, it is suggested that you speak with a podiatrist who can successfully treat this condition.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Rahil Baxamusa, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
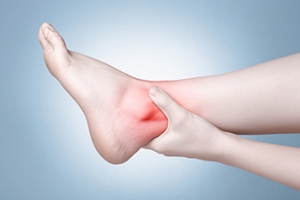
Causes of Ankle Pain

Ankle pain can affect the ability to complete your daily activities and in some cases, if left untreated can develop into a chronic condition. The main causes of ankle pain include sprains, arthritis, and Achilles tendonitis. Other causes are gout, damage to cartilage, and fractures. If you have broken an ankle bone, seeking immediate medical attention is a must. Other symptoms that indicate a trip to the podiatrist include the inability to bear weight, a deformity developing on the ankle, and pain occurring at night or while the ankle is at rest. Further indicators are pain that persists over a few days, trouble bending the ankle joint, swelling into the calf area, or signs of infection. Treatment options for ankle pain are dependent on the cause and can range from rest to surgery. In many cases, changes in footwear and wearing a brace or other orthotic device will be necessary. Specific stretching exercises and types of medication can help to relieve the pain. If you believe you have injured your ankle, it is suggested that you make an appointment with a podiatrist for an exam and appropriate treatment.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Rahil Baxamusa, DPM from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
The ankle joint is the point at which the bones of the leg and foot join. This joint is crucial because it is responsible for the foot’s mobility. Ankle pain is typically the result of inflammation from an injury to bones, joint space, cartilage, ligaments, tendons, or muscles in the area. Commonly associated symptoms with ankle pain are bruising, redness, numbness, stiffness, weakness, and tingling.
The most common causes of ankle pain are sprains and injuries. Ankle sprains are one of the most common musculoskeletal injuries. Sprains occur when the ligaments of the ankle become partially or completely torn due to sudden stretching. Sprains can occur on either the inner or outer sides of the ankle joint. Usually, these injuries occur when the ankle is twisted in an activity by stepping off an uneven surface. More specific causes include rheumatoid arthritis, gout, osteoarthritis, and Achilles tendonitis.
If you are experiencing ankle pain, you should consult with your podiatrist to choose the best method of care. Your doctor will conduct an examination of your ankle to determine the underlying cause of the pain.